Urologic Cancer Surgery
Urologic cancer surgery involves careful decision-making, not automatic intervention. This section explores the surgical management of prostate, kidney and bladder cancers, including when surgery is appropriate, when surveillance is safer, and how outcomes are influenced by tumour biology, anatomy and patient priorities. The focus is on clarity, judgement and realistic expectations — before, during and after treatment.
Age changes the context of cancer care. This article explains how surveillance and treatment decisions evolve as risk, health and priorities shift over time.
Living with cancer on active surveillance can feel harder than expected. This article explores the practical and emotional realities, and how patients are supported over time.
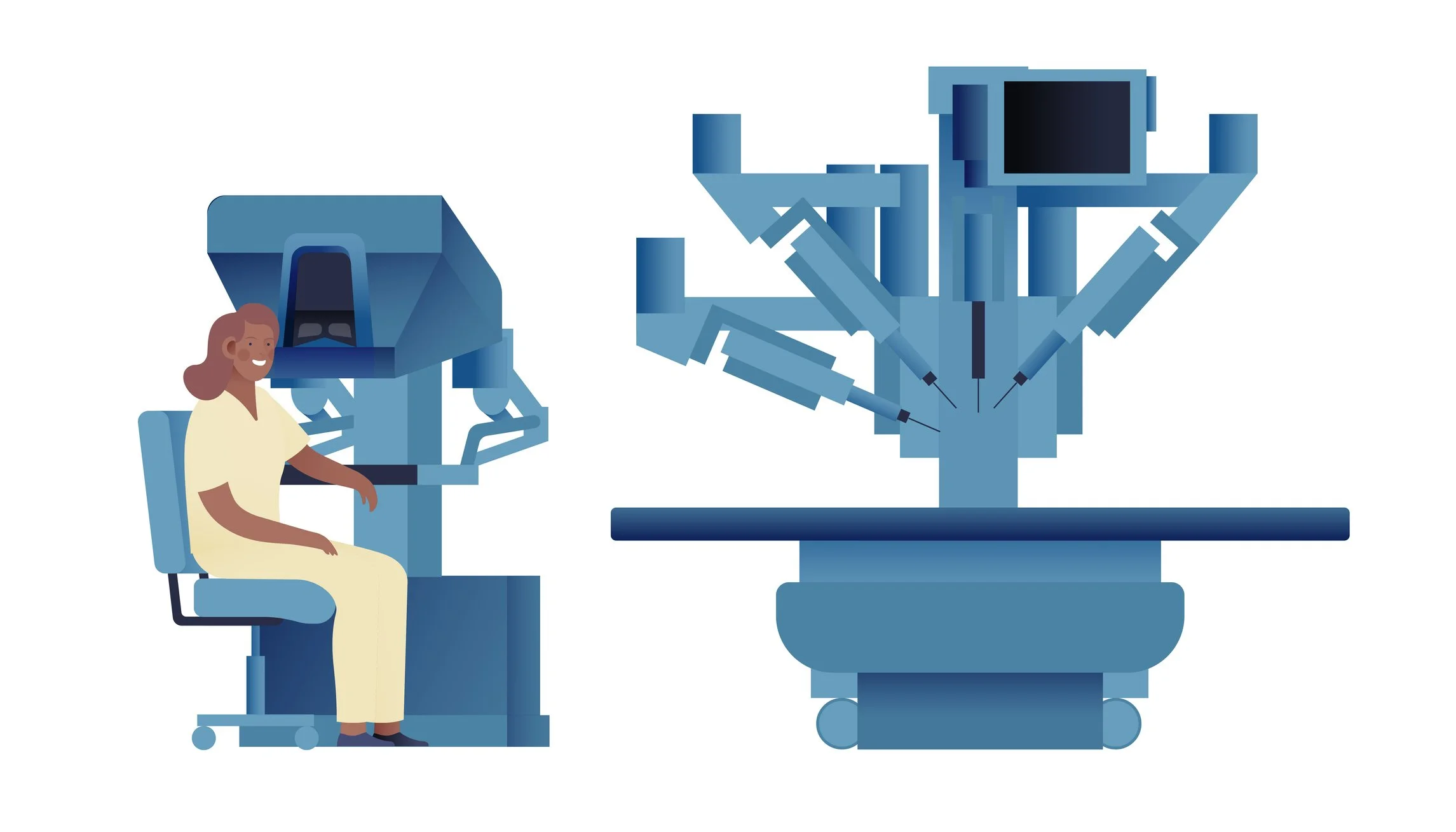
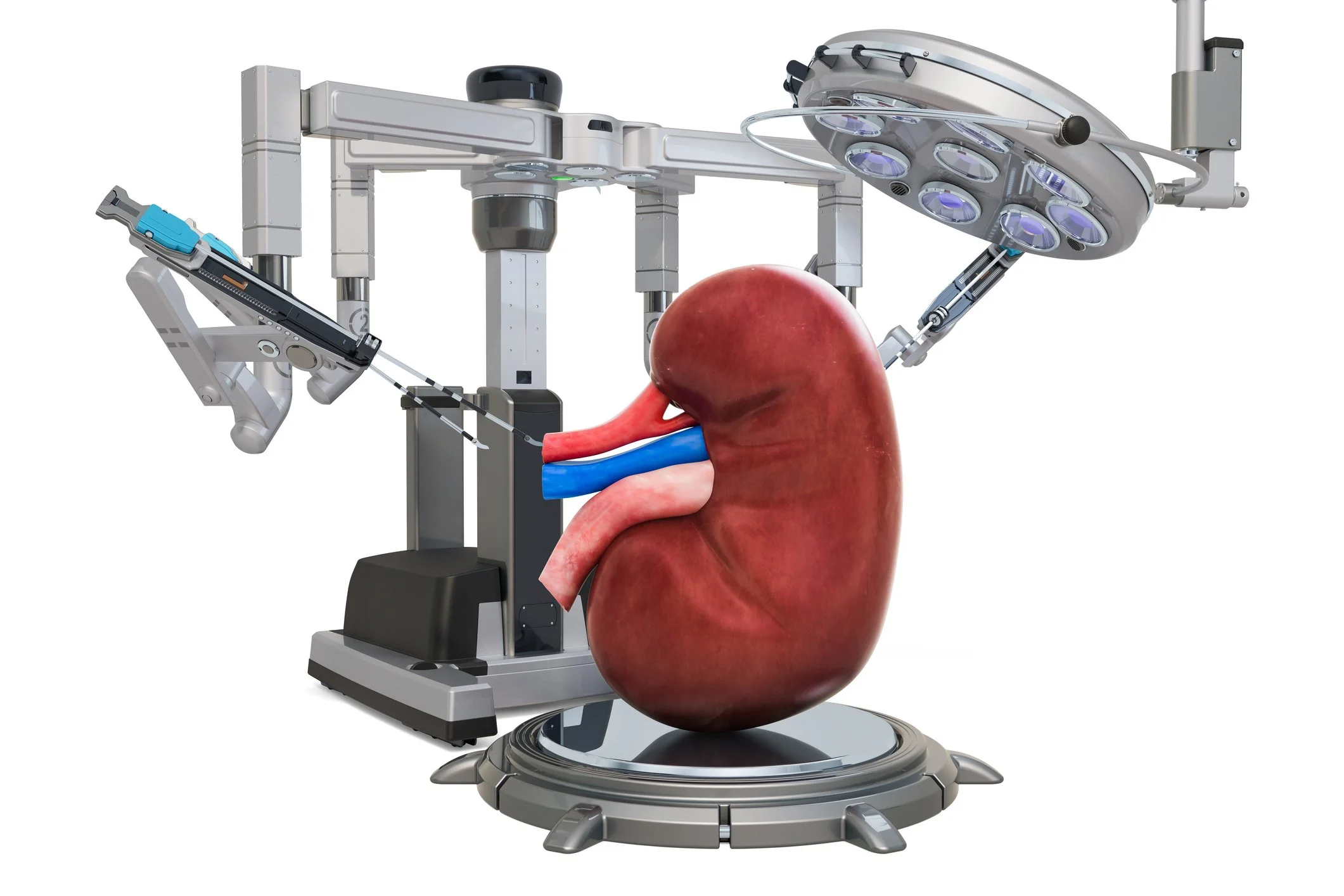
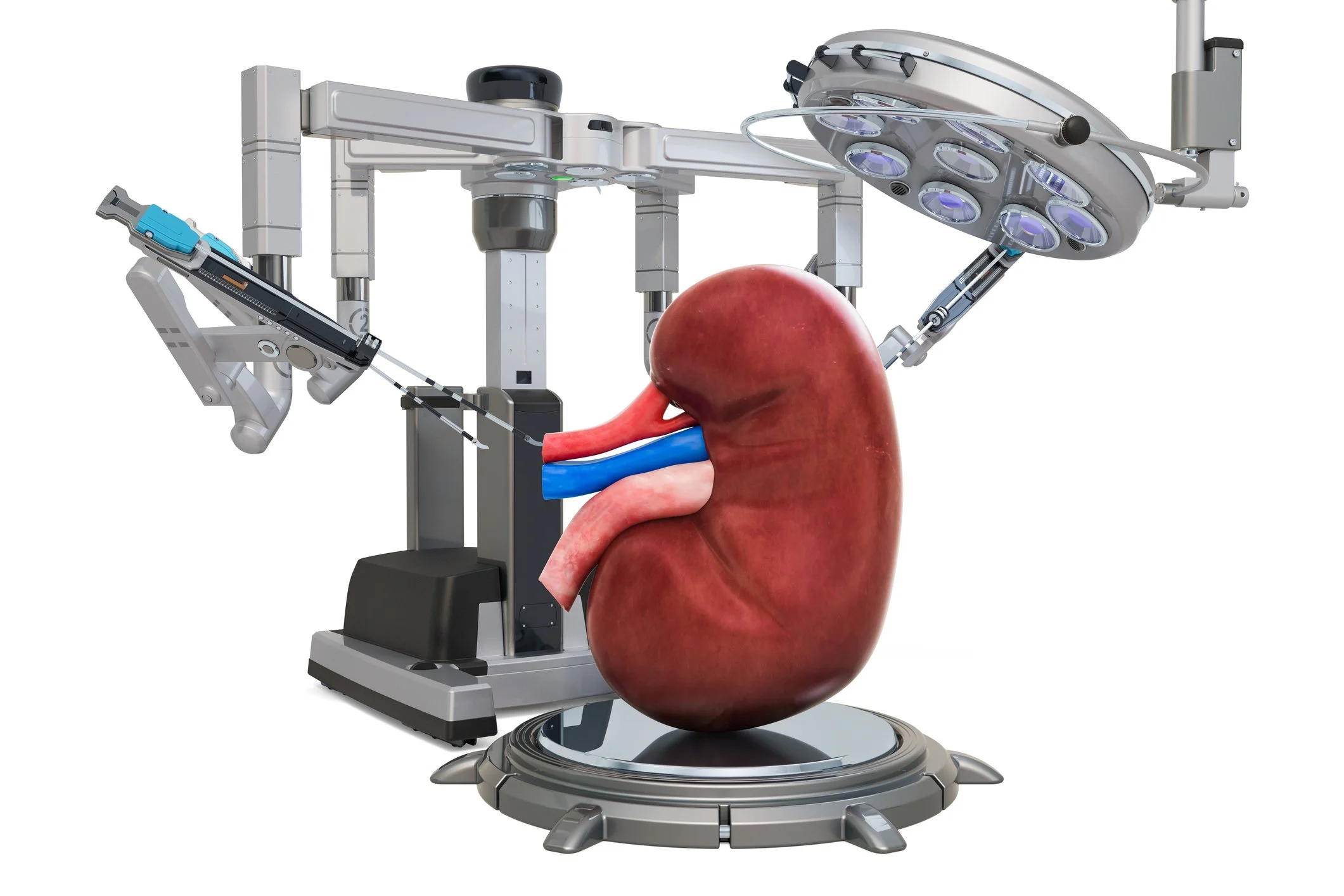
Robotic surgery is a tool in kidney cancer care — not the treatment itself. This article explains when robotic surgery helps, when it doesn’t, and how decisions are really made.
An honest overview of life after radical cystectomy, including recovery, urinary diversion, emotional adjustment and how patients and families adapt over time.
Active surveillance can be the right choice for selected urologic cancers. Learn when monitoring is appropriate, how risk is assessed, and what follow-up involves.
Recovery after robotic cancer surgery is rarely linear. This article explains what patients often underestimate about fatigue, function and emotional adjustment.
An overview of modern bladder cancer surgery, from transurethral procedures to cystectomy, explaining when each approach is used and why decisions are staged.
Positive margins and rising PSA after prostate cancer surgery are common and often misunderstood. This article explains what they mean and how salvage treatment decisions are made.
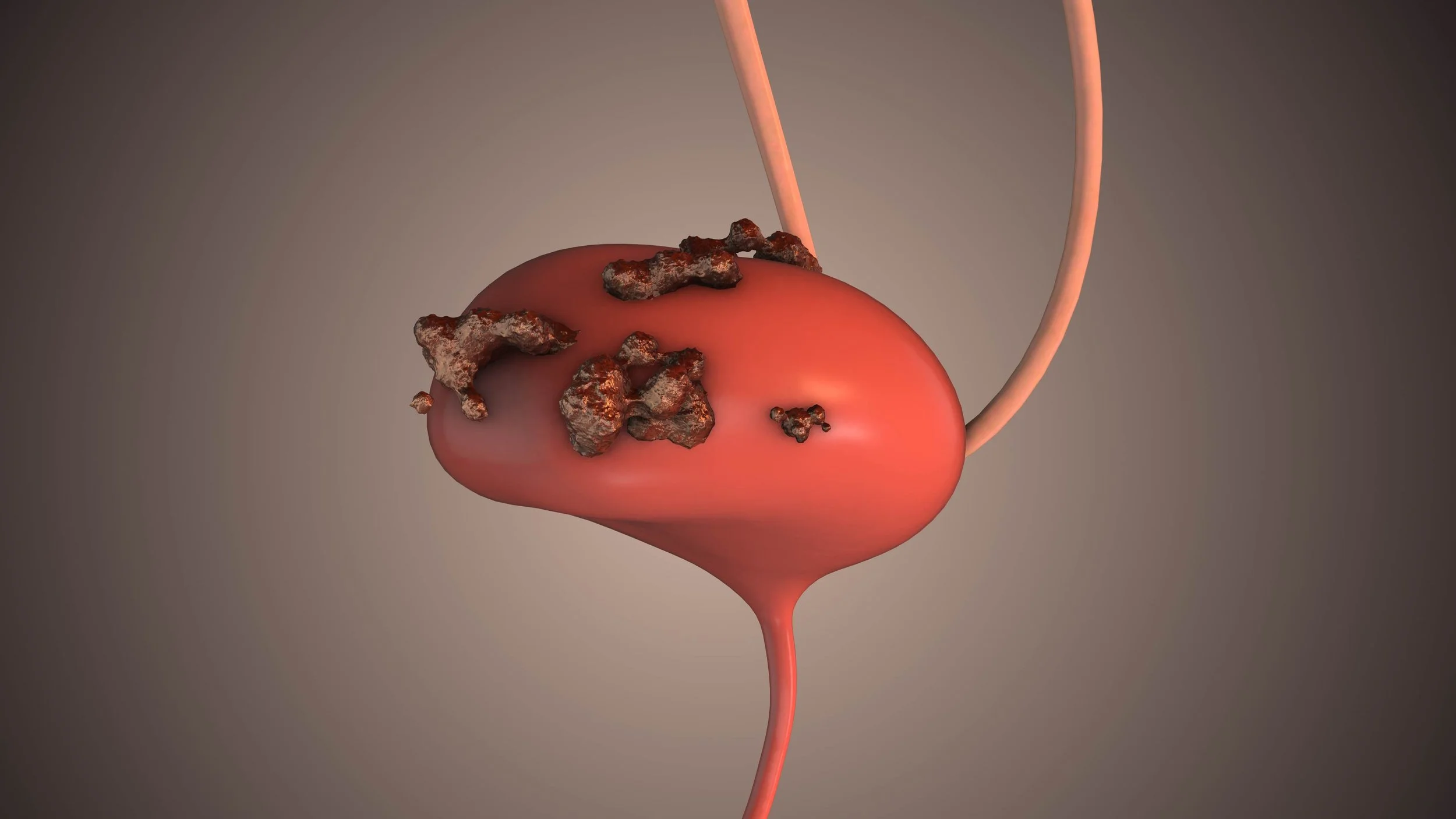
One of the most important decisions made in kidney cancer surgery is not whether to operate, but how much kidney to remove.
Patients are often told they need “kidney surgery” and understandably assume the choice is straightforward: remove the tumour, remove the kidney, move on. In reality, the decision between partial nephrectomy (removing the tumour while preserving the rest of the kidney) and radical nephrectomy (removing the entire kidney) is one of the most nuanced judgement calls in urologic oncology.
Not all kidney cancers require immediate surgery. This article explains when surgery is recommended, when surveillance is appropriate, and how decisions are individualised.
How surgeons decide between partial and radical nephrectomy in kidney cancer, balancing oncological safety with long-term kidney health.
Surgery and radiation are both valid treatments for prostate cancer. Learn how decisions are made, what factors influence recommendations, and how care is individualised.
Many write about robotic prostatectomy as though the robot itself is the story. Learn what actually drives outcomes — oncologic control, nerve sparing, surgeon judgement and recovery realism.
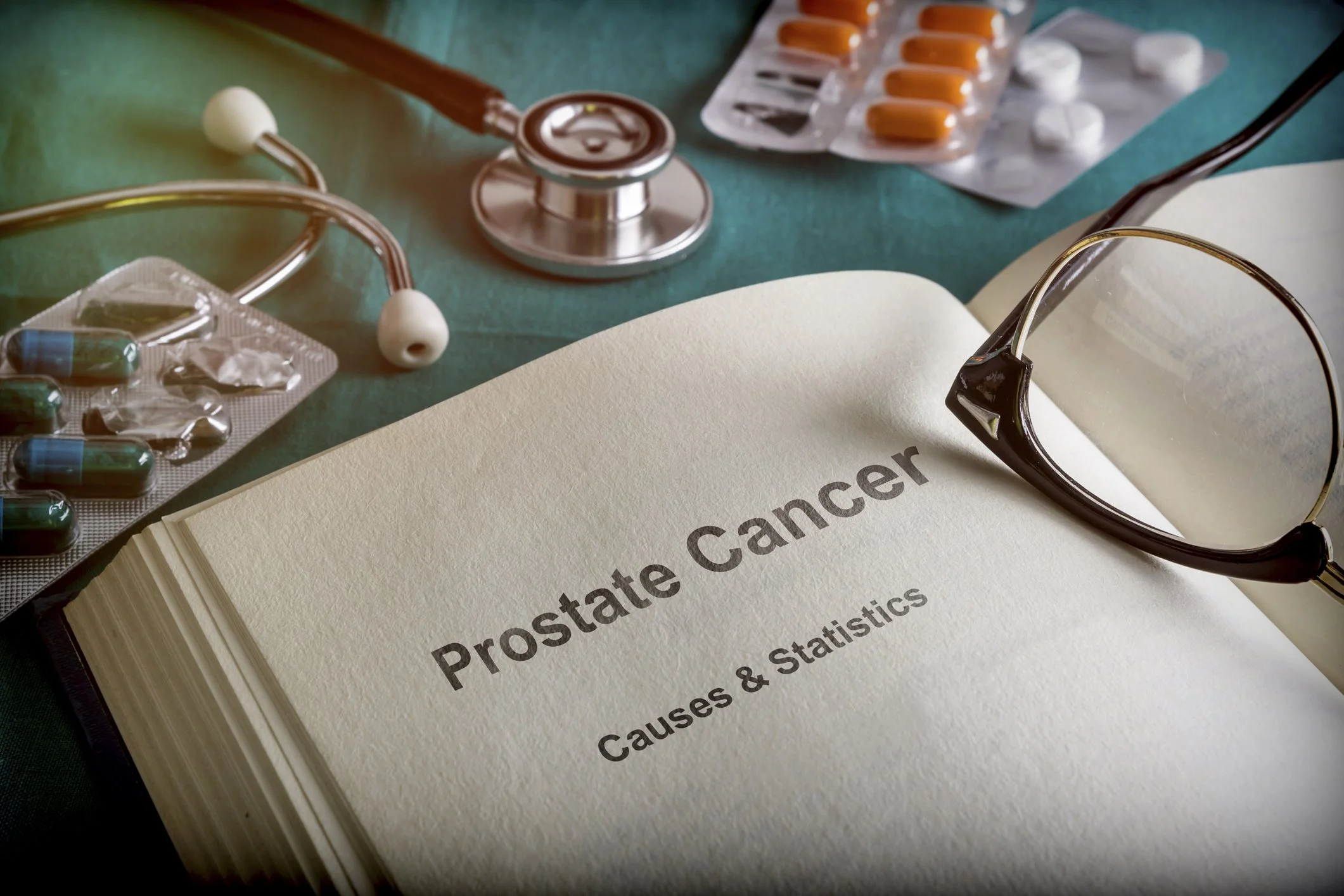
Facing a prostate biopsy may seem overwhelming at first, but understanding the procedure, its purpose, and what to expect can make the experience easier to manage. This guide will provide a detailed explanation of the reasons for a biopsy, the different types available, what you can expect during and after the procedure, and what the results might indicate.
Prostate-Specific Antigen (PSA) testing is one of the most important tools we have for monitoring prostate health and detecting potential issues early. If you've been told you need a PSA test, or you're trying to understand your results, this comprehensive guide will help you navigate everything you need to know.
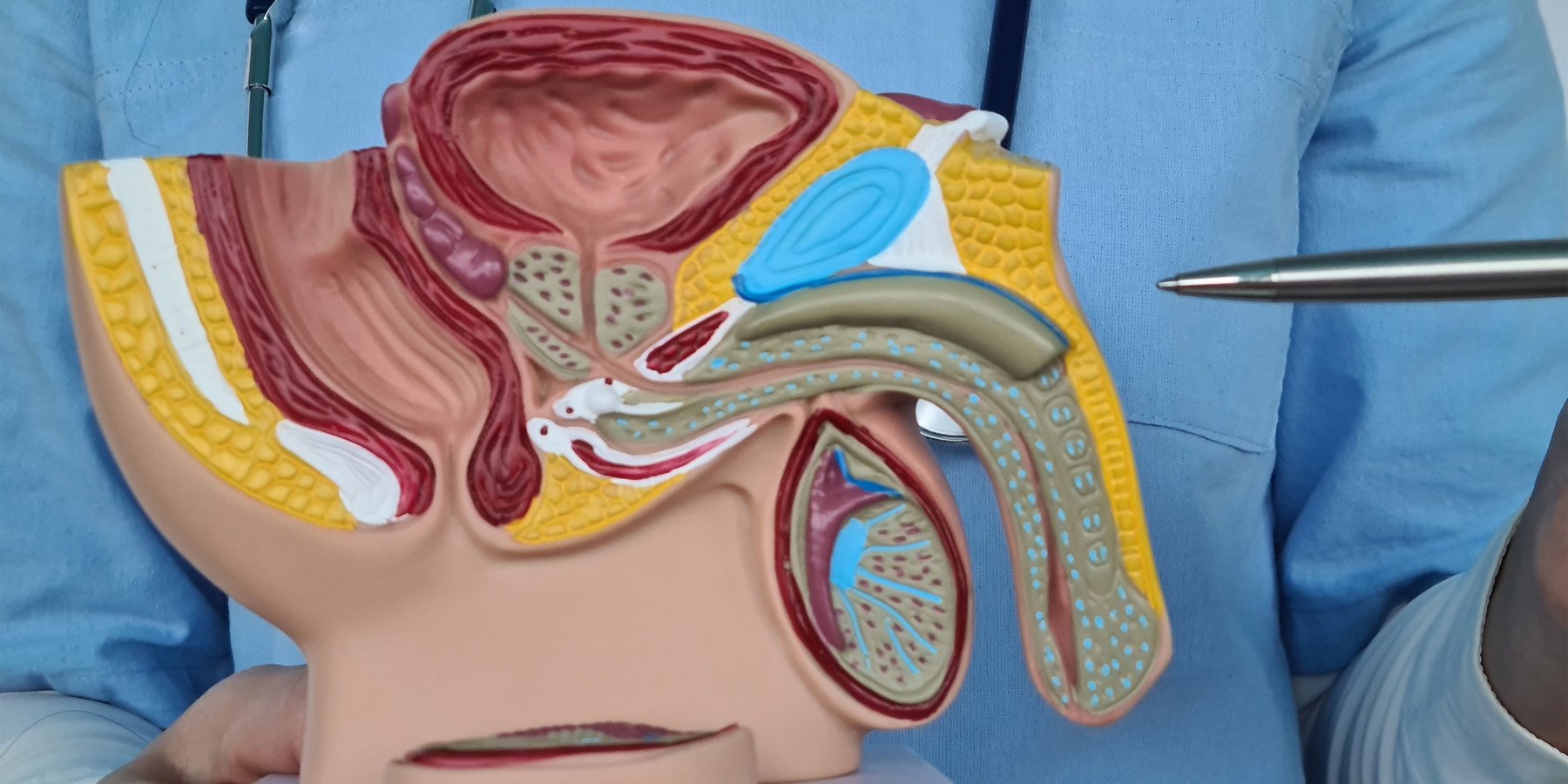
Prostate surgery is a necessary step in managing localised prostate cancer. However, it can significantly impact a man’s sexual health and overall quality of life. One of the primary concerns following this procedure is the effect on erectile function, typically due to the involvement of the nearby nerves that control erections. However, with advancements in surgical techniques, such as nerve-sparing approaches, and strategies for recovery, there is hope for patients to regain function and improve their overall health.
Prostate Cancer surgery is a life-altering event. While the surgery itself focuses on improving or maintaining your health, it can bring about unexpected changes when it comes to intimacy and pleasure. For many men and their partners, the prospect of maintaining a fulfilling sexual connection after surgery can feel uncertain.
Prostate Cancer Surgery in often the main treatment for localised prostate cancer. While the decision to undergo surgery is an essential part of the treatment process, understanding the recovery process is equally critical. For prostate cancer survivors, caregivers, and healthcare professionals in Australia, this guide provides insight into the recovery timeline, the adjustments patients may need to make, and tips for navigating this phase with confidence and care.
Testicular cancer occurs in the testicles, which are part of the male reproductive system. It typically affects younger men, often those between the ages of 15 and 35. Despite its rarity, early detection and treatment can lead to high success rates. Learning about this form of cancer helps in recognising symptoms early, which is crucial for effective treatment.
Prostate cancer is one of the most prevalent cancers among men and people with prostates in Australia, posing unique challenges related to its early diagnosis and effective management. Understanding the intricacies of prostate cancer begins with a thorough knowledge of its origins, risk factors, and development.